Wisdom Teeth
What are wisdom teeth?
They are the third molars and the last teeth to emerge at the back of your mouth. This usually occurs in late teens (‘the age of wisdom’). Most people have four, two in the upper jaw and two in the lower jaw.
Why am I having mine removed?
Surgical removal can be required for several reasons. Often, wisdom teeth get stuck (‘impacted’) against the adjacent tooth or within the jawbone and are not able to come through fully into the mouth.

A partially exposed wisdom tooth can be difficult to keep clean. This can then cause chronic infection and discomfort in the surrounding gum tissue. Such infections may require treatment with antibiotics.
A wisdom tooth can also become decayed or cause decay in neighbouring teeth. Your dentist may not be able to treat this decay until the wisdom tooth has been removed.
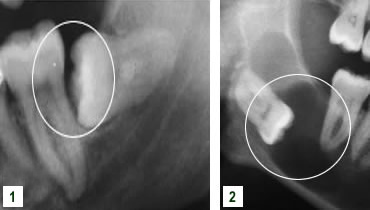
Decay Example
- Extensive decay affecting upper and lower impacted wisdom tooth.
- Impaction of lower wisdom tooth leading to development of decay in the lower second molar.
- Extensive decay affecting impacted lower wisdom tooth.

Impacted Wisdom Teeth
Impacted wisdom teeth can also adversely affect the attachment of adjacent teeth or be associated with cystic lesions.
- Horizontally impacted wisdom tooth adversely affecting attachment of second molar.
- Extensive cystic development around impacted lower wisdom tooth.
Wisdom teeth should only be removed if they are causing problems. We will discuss this with you during your appointment.
How will it be removed?
This depends on the position of your tooth and the way it is impacted. Some wisdom teeth can be quite straightforward to remove but more commonly simple extraction is not possible and surgery will be required to remove it.
The nature of this surgery depends on the position of the wisdom tooth. This may influence whether your operation is carried out under local anaesthesia alone or with additional intravenous sedation.
All options can be discussed with you during a consultation appointment.
How long will the operation take?
This depends on the position of your tooth or teeth and whether the operation is being carried out with local anaesthesia alone or with additional intravenous sedation. An appointment for surgery under local anaesthesia usually lasts 60 minutes.
When intravenous sedation is used an appointment usually lasts 90 minutes; this longer time allows for the recovery period needed before you can be discharged home.
Will there be any stitches?
Stitches are usually required as part of these procedures and will be dissolvable. These stitches can take up to 2 weeks to go although sometimes they break down much sooner.
Will I be in pain afterwards?
You should not feel any pain immediately after the operation as the area of surgery will be numb from the local anaesthetic. As this numbness wears off the area might become uncomfortable and you should then take painkillers. We will supply you with these together with information about doses.
Could there be any after-effects?
This depends on the nature of your operation; if there are any issues in particular to be aware of this will be discussed with you beforehand. Your dentist will have supplied a standard x-ray image of your tooth/teeth but sometimes a more detailed 3-D view will be required using a cone beam computed tomography (CBCT) scan. The findings of this imaging will be discussed during your consultation.
There may be swelling, bruising and discomfort in the area of the surgery together with some limitation in jaw opening. The bruising is usually at its most obvious 2 to 5 days after the procedure and will vary between patients; it normally resolves after 7 to 10 days.
Occasionally an impacted lower wisdom tooth can be very close to the nerves that carry sensation from the lower teeth, lip, cheek and chin and sensation/taste from the tongue. These nerves can get bruised when the tooth is removed, leading to tingling, numbness, altered taste or pain in these areas.
These changes in sensation only affect 2-5% of patients and are usually temporary. They can take up to 6 months to fully resolve and only very rarely become permanent. If this is a factor for you to be aware of due to the proximity of your wisdom tooth to these nerves we will discuss this with you during your consultation.
The roots of upper wisdom teeth can be very close to the air space (antrum) within the cheekbone leading to the risk of a communication developing between this air space and the mouth following the removal of such a tooth. The likelihood of this can be very much reduced by avoiding vigorous sneezing or nose blowing for the first 2 to 3 weeks following the procedure.
Coronectomy procedure
A coronectomy procedure aims to remove the top part of the tooth which is causing problems and leave the rest of the tooth in place within the jaw bone.
This procedure might be suggested if there are concerns that removing the whole tooth could result in damage to the nerve that carries sensation from the lower teeth, lip and chin leading to tingling, numbness or pain in these areas.
A coronectomy procedure might not be suitable if the tooth is decayed or if there is infection around its root. In those circumstances it will be suggested that the whole tooth is removed.
The side effects from a coronectomy procedure are similar to the removal of the whole tooth including the potential for bruising affecting the nerves that carry sensation from the lower teeth, lip, cheek and chin and sensation/taste from the tongue on the side of the procedure leading to tingling, numbness, altered taste or pain in these areas.
These changes in sensation only affect 1-2% of patients and are usually temporary. They can take up to 6 months to fully resolve and only very rarely become permanent.
As the tooth root has been left in place there is a risk of this causing infection at the operation site. The root might also move slowly over time and sometimes start to appear in the mouth. In both cases the root might need to be removed (approximately 15% complication rate).
When can I return to work?
This depends on your occupation and how you are after your treatment. It may be possible for you to return to college or work the next day but some people will need to take some time off especially if the operation has been carried out under intravenous sedation. We will give you appropriate advice for your particular circumstances.
Postoperative advice
Find out how to help bring about a quick recovery after an operation.
